“What is a Transperineal Prostate Biopsy?” you might ask. This advanced outpatient procedure is distinct from traditional transrectal methods, requiring a deeper level of anesthesia for utmost precision and patient comfort. During the biopsy, an anesthetic is applied to the perineum, which might cause a brief sting. Following this, the doctor employs an ultrasound probe to visualize the prostate on a screen, ensuring accurate placement of the biopsy needle. It’s worth noting that incorporating prostate antioxidants in one’s regimen can be beneficial for overall prostate health and recovery after such procedures.
What is the procedure?
Under general anaesthetic, your physician will conduct the biopsy through skin behind your testicles (known as the perineum) under local anaesthesia. Antibiotics will also be provided prior to beginning this procedure, to reduce any risk of an infection occurring during or following it.
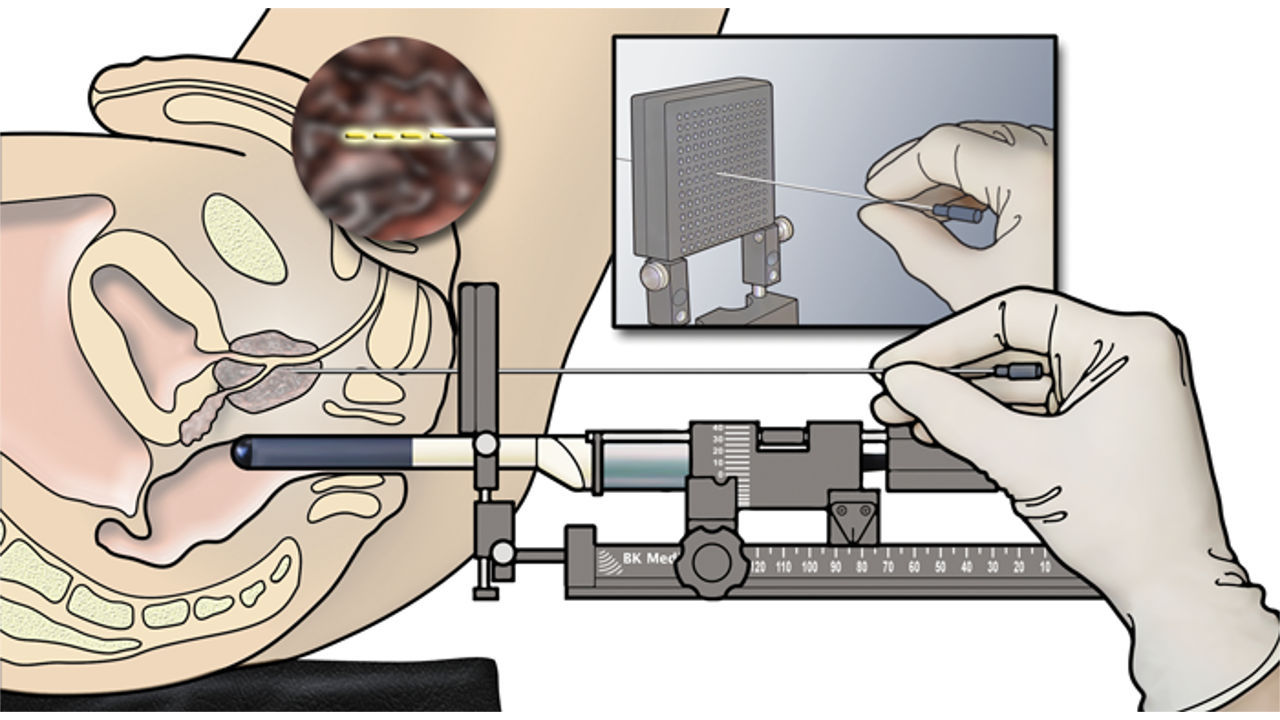
Your doctor will use an ultrasound probe held in a stepper to visualize your prostate, while a fine needle is then used to collect multiple tissue samples from various areas such as its apex and anterior regions. This approach allows your physician to sample more of the prostate while more easily accessing those areas that might otherwise be difficult.
After your biopsy, a catheter will be placed into your bladder to drain urine for several days at home. Some men may find it hard to urinate post-biopsy due to swelling of their prostate gland; if this is the case for you, your doctor will ensure you can urinate before sending you home from hospital and may suggest you use one as part of a temporary solution for drainage at home if necessary.
If cancer is discovered in your prostate it will be classified using Gleason scores and grade groups to indicate its likelihood of growing and spreading; lower scores indicate less aggressive cancer cells.
What are the risks?
Transperineal prostate biopsies are used to identify cancer cells in the prostate. When your PSA or digital rectal examination identifies potential concerns, your doctor inserts a needle through your perineum skin into the prostate to collect tissue samples for laboratory analysis – you’ll typically undergo this test under local anaesthetic, although sometimes general anaesthetic is also available for this procedure.
Urologists with experience conducting transperineal prostate biopsies can perform this procedure, explaining both its risks and benefits in detail when first referred. On biopsy day itself they will also provide contact numbers of specialist nurse support to answer any inquiries that arise during or after.
As part of your biopsy preparation, antibiotics will be provided to you to help prevent infections afterward. They must be taken for several days following your test, although some men may experience temporary issues urinating (voiding) following this type of exam; these side effects usually fade over time.
After your biopsy, it is normal to experience some temporary discomfort or bruising at the site where the needle went in for several days post-procedure. Furthermore, small amounts of bleeding might occur in your back passage or bowel and you might need to visit A&E in severe cases.
What are the benefits?
A prostate biopsy uses thin needles to collect samples of tissue from your prostate to look for cancer cells under a microscope, before sending the samples off to be analysed by laboratory technicians for signs of cancer. You may receive this examination in either an outpatient department or operating theatre setting under general anaesthetic.
Traditional biopsies are done using transrectal ultrasound-guided (TRUS) techniques. This requires inserting a needle through the back passage (rectum) into the prostate. Unfortunately, there is an increased risk of serious infection using this approach; bacteria could enter through any holes in the rectal wall into bloodstream resulting in what’s known as “septicaemia.”
Transperineal biopsies enable your urologist to use information from an MRI scan as guidance when taking the biopsy needle from its sheath and placing it. This reduces needle punctures and thus the risk of complications; additionally, this approach lowers infection risks as the needle won’t need to pass through an area such as perineum that could harbor bacteria.
Some men may experience discomfort during this procedure; should this occur, your nurse or doctor will provide pain-relieving medications if necessary. If you experience any difficulties passing urine or having bowel movements that contain large quantities of blood, immediately speak with either of them about it.
What are the alternatives?
Doctors may use blood tests and prostate-specific antigen (PSA) levels to help determine whether you require a biopsy. But these tests cannot yet replace having one performed, which provides the best way of checking PSA levels, types and numbers of cancer cells as well as their potential to grow or spread.
Some men experience intense discomfort following a biopsy, while other may only feel mild discomfort. Should any discomfort arise, your nurse or doctor will provide pain-relief medication as necessary.
Before taking biopsies, your doctor can look over your MRI scan results and decide where they want to perform biopsies. They may take targeted biopsies in areas where they suspect cancer; otherwise they may take systematic biopsies from other parts of your prostate gland.
Temporarily, having a transperineal biopsy or template biopsy could cause temporary problems urinating due to needle getting closer to your urethra which runs through your prostate gland and more samples being taken by doctors. You might need a catheter at home for several days in order to drain urine out of your system.