When it comes to men’s health, understanding the intricacies of a prostate biopsy is crucial. Doctors performing prostate biopsies meticulously collect tissue samples from different regions of the gland, analyzing them under a microscope to search for the presence of cancer cells. Once analyzed, these results are then systematically classified and assigned a Gleason score. This score not only measures how abnormal the prostate cells appear under microscopic examination but also provides valuable insights into the potential growth and spread of cancer, if present. But how do you decipher these findings? Delving into “how to interpret prostate biopsy results” is essential for a comprehensive understanding. Moreover, it’s equally vital to know what are the after effects of a prostate biopsy, when to take enema before prostate biopsy, and what not to eat before prostate biopsy to ensure both accurate results and a comfortable recovery.
Understanding Prostate Biopsy Basics
For the most common type of prostate biopsy, a physician inserts a needle through your rectum into your prostate and extracts cores for laboratory analysis. Once these cells arrive at their destination, a pathologist examines them closely under a microscope and writes their diagnosis onto the biopsy report.
Doctors may use ultrasound or magnetic resonance imaging (MRI) to guide a biopsy needle. Ultrasound works by inserting an ultrasound tool into your rectum and producing an image of your prostate that helps guide biopsy needle placement. Meanwhile, with MRI they can examine it more in-depth than ultrasound could ever allow; some doctors also combine both techniques together for something called template biopsy – using software as guidance for needle placement.
Men should consult their doctors about obtaining a template biopsy. While this does not increase their odds of receiving an incorrect Gleason score or grade group diagnosis, which could impact treatment recommendations.
What is the Gleason Score?
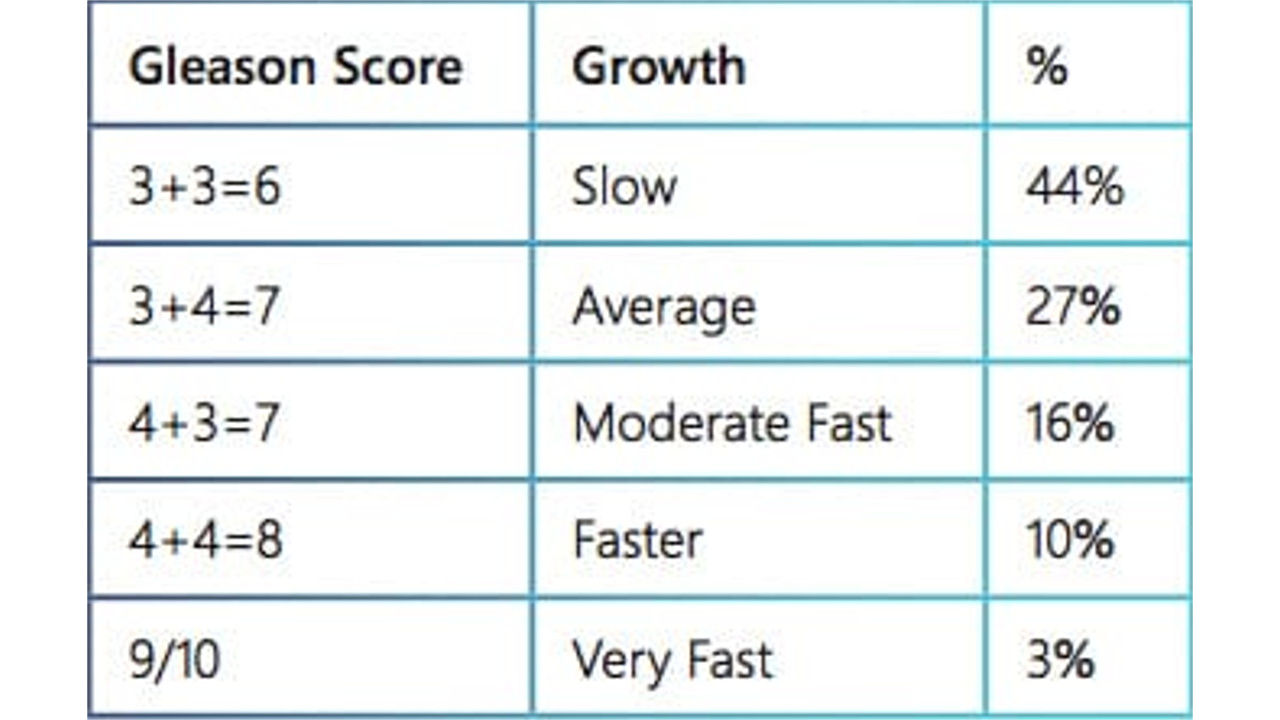
Healthcare providers take many factors into account when developing your treatment plan, including Gleason scoring system that evaluates how similar cancer cells look to healthy prostate tissue. Lower Gleason scores indicate less likely spread.
Doctors evaluate tissue samples obtained during a biopsy by viewing them under a microscope and assigning numbers for patterns they identify; they then combine scores from two of the most frequent patterns within your sample (for instance 3 + 4).
Your prognosis will also depend on your Gleason score and other factors, including any evidence of perineural invasion (cancer cells found growing near nerves). If your Gleason score falls into one or two groups, doctors may advise active surveillance or non-treatment options while for Gleason scores that fall in groups 4, 5 or 6, treatment will likely need to begin earlier and further diagnostic tests may be ordered to gauge its aggressiveness.
Distinguishing Benign from Malignant Findings
Your doctor will collect a small sample of cells from your prostate using ultrasound probe or MRI scanning technology to pinpoint where to collect samples. In addition, molecular-based tests may help doctors recognize how aggressive cancer cells are by comparing them to normal prostate cells and predicting how likely they will spread further.
Pathology reports will also include an account of the tissue involved. They will explain whether core or saturation biopsy was conducted and from where samples came (i.e. apex, mid zone or base). They also detail how much of prostate tissue is included per sample and how many cells exist within.
Pathologists examine biopsy samples under a microscope to check for cancerous cells. When results are inconclusive, the pathologist may state that they suggest or suspect cancer but cannot make a definitive diagnosis – something men are left frustrated about as it means their doctor might have found enough cells that indicate cancer but cannot give an exact diagnosis.
What is Small Acinar Proliferation?
Although morphologic criteria have become increasingly accurate over time, there remains a small percentage of prostate biopsy specimens with foci that meet qualitative or quantitative criteria but fall below an accepted diagnostic threshold; these cases are known as Atypical Small Acinar Proliferations (ASAPs).
Cool et al analyzed 36 patients diagnosed with ASAP at Yale-New Haven Hospital who received their diagnoses through pathology reports; in half of these instances the term ASAP was included as either the principal diagnostic line or note in their pathology reports, respectively. In one of their studies they observed that term ASAP appeared either in its principal diagnostic line or note portion of pathology reports in each instance – although notably only once appeared as part of its principal diagnostic line in its report!
The authors advise physicians to consider performing a second biopsy on patients diagnosed with ASAP, since their study revealed an elevated incidence of cancer at second biopsy for those diagnosed with ASAP. Other predictors for cancer at repeat biopsy include multiple atypical cores, high grade prostatic intraepithelial neoplasia (HG-PIN), or cores showing glandular atypia in multiple locations.
Importance of Pathology Reports
Pathology reports provide your doctor with a thorough look at the tissue from your biopsy sample, providing them with vital insight into the severity and spread of prostate cancer. They detail Gleason scores and how many cores in each biopsy contained cancer; additionally they outline whether cancer was located on either side or both; whether in its apex, mid zone or base region.
Your pathology report will also detail what type of prostate cancer you have (acinar adenocarcinoma or transitional adenocarcinoma). As the type can influence its aggressiveness, it is crucial for doctors to know exactly which kind of prostate cancer you have so they can determine suitable treatments options.
Prostate Cancer Staging and Grading
Your biopsy report will inform you if there is cancer present and its type and extent. In addition, its stage, whether or not it has spread nearby such as bladder or rectum tissue or other parts of your body such as bones can also be included as part of this information.
Pathologists examine prostate cells under a microscope and grade them according to how different they look from healthy prostate cells. If cancerous ones look far different from normal, they’re considered more aggressive and are given a score between 1-10; doctors will then combine the highest two scores for an overall Gleason score.
Doctors also employ another, simpler system called Grade Group that makes cancer risk easier to assess and understand for patients. It combines data such as PSA levels and tumor size to give a full picture of risk categories for cancer treatment.
Potential Risks and False Results
At a biopsy, doctors insert a needle into your back passage (rectum or perineum) and take out a small cylinder of tissue from your prostate gland for testing by pathologists specializing in diagnosing cancer and tissue abnormalities under microscope to assess whether or not there are cancerous cells present and their potential aggressiveness.
If the test indicates cancer cells, your doctor will assign you a Gleason score and grade group. These grades indicate how abnormal the cells look under a microscope as well as their likelihood of growing and spreading beyond your prostate.
Pathologist might also note atypical or suspicious cells within your sample. While these abnormal cells could later lead to cancer diagnosis, they’re insufficient evidence right now; nevertheless, your doctor might still recommend treatment, while repeat biopsies might give more definitive results.
Next Steps After Receiving Biopsy Results
Reading your pathology report is essential to properly discussing its results with your physician or nurse, so bring along someone from your family or an acquaintance for support and notes during this discussion.
Pathology reports will outline what kind of cancer was found in biopsy samples and its propensity to grow and spread, along with giving a Gleason score or grade group (lower scores or grades indicate greater chance that cancer spreads).
Sometimes a biopsy sample contains “atypical” cells, which appear suspicious but the pathologist cannot definitively state whether or not they are cancerous. This situation is known as an “equivocal diagnosis”, and can be both confusing and distressing for you and your physician.
How a prostate biopsy is conducted can have a dramatic impact on its outcome. Before your hospital performs the biopsy, find out their method for preparing the samples to view under a microscope; some hospitals place each biopsy core into its own separate labeled container while others combine all cores for processing.
Conclusion
In wrapping up, understanding how to interpret prostate biopsy results is pivotal in the early detection and management of prostate conditions, especially cancer. These results, often relayed through terms like the Gleason score, offer crucial insights into the nature of the prostate cells and the potential threats they might pose. Armed with this knowledge, individuals can collaborate more effectively with their healthcare providers, making informed decisions about their treatment and future health. Staying informed and proactive is the key to navigating the complexities of prostate health.
Frequently Asked Questions
- What does a higher Gleason Score indicate? A higher Gleason Score, approaching the number 10, generally indicates that the prostate cancer is more aggressive. This means the cancer cells are less like normal cells and may spread more rapidly.
- What is the significance of Perineural Invasion? Perineural Invasion (PNI) indicates that cancerous cells are surrounding or touching nerve fibers within the prostate. This can signify a higher risk of the cancer spreading beyond the prostate.
- How do doctors use the Grade Group? The Grade Group is utilized to predict the aggressiveness of prostate cancer. It complements the Gleason Score and helps doctors determine the most suitable treatment options and prognosis.
- What’s the importance of the gross description in a pathology report? The gross description provides an overview of the biopsy tissue sample’s appearance, such as its color, size, and texture. It gives doctors an initial perspective before delving deeper into microscopic details.
- Are there any side effects after a prostate biopsy? After a prostate biopsy, individuals might experience discomfort and more frequent urination due to prostate swelling. In some cases, a temporary catheter might be required to assist with urine drainage. It’s essential to communicate with your doctor if you’re on medications like blood thinners.