Curious about ‘What Does an Enlarged Prostate Feel Like on Exam’? Positioned below the bladder, the prostate often enlarges with age due to benign prostatic hyperplasia (BPH). Unlike some conditions, BPH is symptom-free and doesn’t raise cancer risks. After discussing symptoms, doctors may seek a blood sample. Prostate vitamin supplements might also be suggested for overall health. Dive deeper now!
Feeling of the Prostate
The prostate gland in men produces some of the fluid used during ejaculation. It’s situated at the lowest part of their pelvis, beneath their bladder that holds urine, in front of their rectum, and surrounds part of their urethra that transports urine between their bladder and penis. Over time, male prostates usually become larger. When this occurs, it’s known as benign prostatic hyperplasia or BPH and doesn’t lead to any symptoms or increase cancer risk in any way.
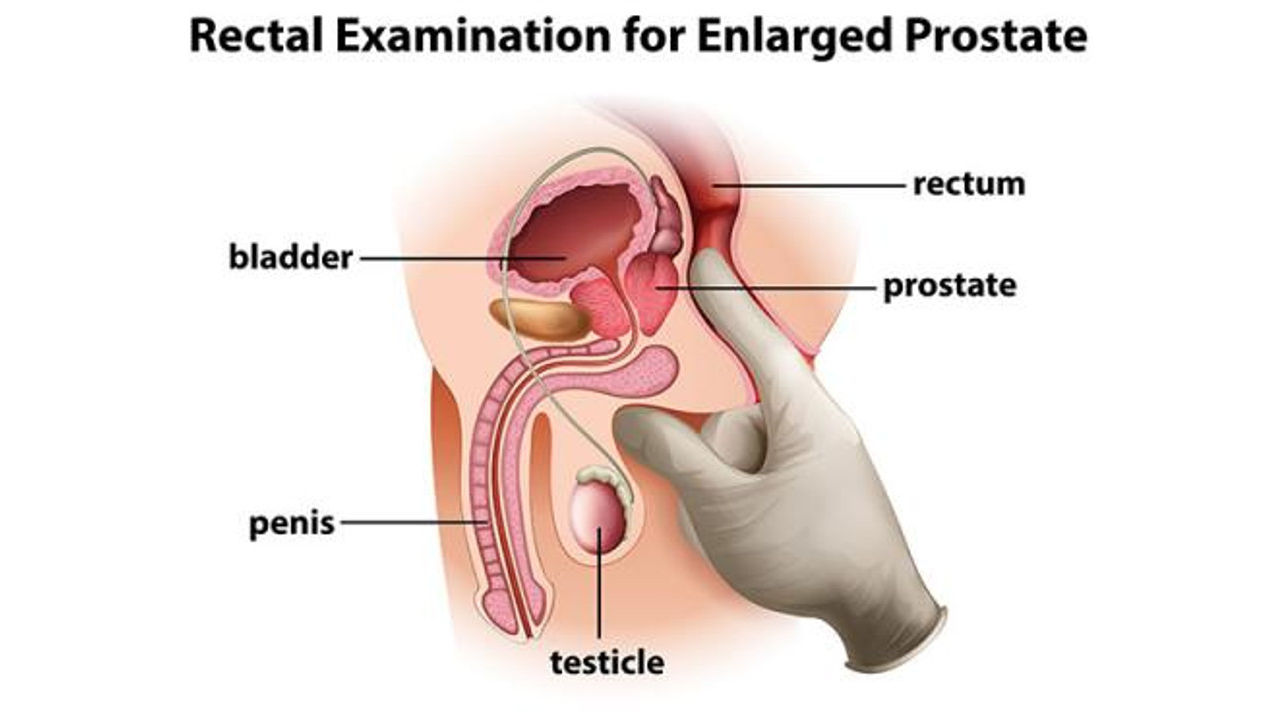
To accurately evaluate your prostate, a doctor or nurse puts on gloves and applies a lubricating gel on their finger before placing their index finger into your back passage and palpating for two lobes that can easily be felt with their finger. A healthy prostate typically feels smooth with two distinct areas easily detected while an enlarged prostate often feels rubbery and hard on contact with their fingertip.
When your doctor feels your prostate, they will ask about symptoms and frequency of urination. They may also check to see if your urine has become cloudy or discolored which could signal infection or request blood tests to measure levels of prostate specific antigen (PSA), which increases when an enlarged prostate grows; an elevated PSA level could signal cancerous growth.
Digital Rectal Examination (DRE)
Health care providers usually wear gloves and apply a small amount of water-based lubricant to their finger, which they then slide inside the patient’s back passage in order to feel the prostate from its rectum. This procedure typically only lasts a few seconds without causing physical injury.
Patients who feel embarrassed or uncomfortable during their exam should notify their healthcare provider immediately, so an alternative test can be administered if necessary. Healthcare providers should be sensitive to patients’ feelings and strive to make the experience as pleasant as possible by explaining that this form of touch is clinically necessary.
As part of a DRE exam, providers may detect whether a man’s prostate has become enlarged and feels lumpy or hard, which are signs that BPH has progressed into more advanced stages. This is an invaluable finding that could indicate further treatment or intervention may be needed for the condition.
At a DRE exam, health care providers will also assess the position of the urethra and anus as well as any swollen veins (hemorrhoids). With this information in hand, the doctor can decide whether more testing is required; options could include PSA tests, an MRI of the prostate or biopsies whereby hollow-core needles are inserted into growths to remove samples for further analysis.
Urinary Tract Insturction (UTI)
The prostate gland, located near the front of the bladder and near to urethra, plays an integral part in men’s lives by producing semen. While usually not very large, as we age our prostates may become larger and press against either bladder or urethra reducing or restricting urine flow – known as benign prostatic hyperplasia or BPH.
BPH may not increase your risk of prostate cancer, but it does increase your chance of UTIs or weak or incomplete urine streams that dribble after you urinate, as well as urinary system infections and pain in the suprapubic region or pelvic region.
Health care providers will discuss your symptoms and how they affect daily life before performing a physical examination of both your stomach and genital area. This exam includes watching you urinate to detect any urinary abnormalities as well as performing a digital rectal examination (DRE), in which a provider inserts gloved fingers into your rectum to feel its back wall for any signs of enlargement, tenderness, or hard spots – making this short exam very important.
If lifestyle changes don’t help, your doctor can suggest minimally invasive surgical procedures to reduce the size of your prostate and alleviate urinary symptoms. One such minimally invasive surgery procedure is transurethral prostatectomy (TUMT), in which an electrical tool destroys any enlarged tissues while protecting surrounding urinary tract through cooling systems.
Urinary Cystoscopy
When other exams don’t reveal any issues with your prostate and bladder lining, your doctor may opt for a cystoscopy (cystourethroscopy). It is typically performed outpatient and you will be asked to empty your bladder prior to starting. Your physician will clean out your urethra opening and apply an anesthetic jelly (an anesthetic jelly is placed where urine comes out either at the end of a penis for men or just before vagina for women), before inserting a long flexible tube equipped with light and camera (cystoscope).
Cystoscopes allow doctors to observe inside of both your urethra and bladder lining, as well as insert other tools through it such as biopsy instruments to take tissue samples or treat conditions such as bladder tumors. Blue dye may be injected through this tube in order to improve visibility within both.
After having a cystoscopy exam, it’s common to experience discomfort when peeing and blood in your urine for one to two days afterward. Drink plenty of fluids so this situation resolves quickly – no serious complications should arise as a result! Contact your GP if the discomfort does not go away after 24 hours, or seek emergency assistance as needed from their local emergency department or go directly to an accident and emergency department if required.